Watch Out! Literally - 16 Case Reports of Corneal Rejections Following the \/
If you poke your immune system in the eye with spiky proteins, its your eye on the chopping block
There are a surprising number of case reports where the patient developed an immune reaction against a graft or implant. After all, how many people are there with corneal grafts or breast implants who got vaccinated and then developed an immune reaction against the implant or graft?
A new study came out recently on this subject, Characteristics and Clinical Ocular Manifestations in Patients with Acute Corneal Graft Rejection after Receiving the COVID-19 Vaccine: A Systematic Review.
This study essentially analyzed a few of these case reports to “determine the characteristics and clinical ocular manifestations of acute corneal graft rejection after coronavirus disease 2019 (COVID-19) vaccination”. They included a grand total of “13 articles on 21 patients (23 eyes) with acute corneal graft rejection after COVID-19 vaccination, published between April and December 2021”.
Daniel Horowitz wrote a great piece on this study (I encourage you to read it in its entirety):
Horowitz: New study shows rejection of cornea transplants following COVID vaccination
It was one of the worst human rights violations of the COVID regime, and it’s still going on in most hospitals. Hospitals were de-listing people from organ transplant lists who would not get the COVID shots, no matter how much information came out on how the shots were unsafe and ineffective, particularly among the immunocompromised. From day one, the policy should have been the other way around – kidneys shouldn’t have been wasted on those who got the shots – and now we have the proof.
According to a study published by Japanese researchers last month in the Journal of Clinical Medicine, a number of patients receiving cornea transplants experienced rejections of the cornea tissue following the COVID vaccines. Cornea grafts are considered a much lower-risk transplant procedure than solid organ transplants and tend to have a much lower rejection rate. Which is why the researchers were surprised to find a total of 23 eyes from 21 patients who had undergone corneal graft procedures who experienced rejection anywhere from one day to six weeks following COVID vaccination. In some cases, the rejection occurred suddenly after being jabbed despite the cornea graft having held steady for many years.
Like so many other studies indicating concerning safety signals about the shot, don’t expect any follow-up to this analysis. If our government really cared about safety and science, it would immediately identify these cases of rejected corneal tissue and study them for spike protein and other tissue protein expression markers.
What this study demonstrates is that rather than accusing the unvaccinated recipients of potentially wasting a transplant, we should be studying whether vaccinated recipients might be at higher risk of wasting transplants and whether vaccinated donors run the risk of transferring to the recipients the spike protein through the grafted tissue or in solid organs.
Although the paper has not yet identified a likely mechanism of action causing rejections in eye tissue, Dr. Richard Urso, an ocular specialist, told me he is not surprised that the mRNA expressing the spike would be able to find and inflame tissue that is typically protected from the immune system. “We’re seeing inflammatory markers in tissues that usually don’t receive this protein because the lipid nanoparticles can spread it anywhere in the body. These particles are particularly adept at crossing tight junctions and can deliver the mRNA to parts of the body like the brain and eye. One thing about blood vessels around the eye is that they are covered by pericytes that are full of ACE2 receptors, which makes sense that it would trigger all the pathways for inflammation including natural killer cells.”
Of course, the authors of this new study concluded that “Corneal transplant recipients may require further vaccination, necessitating appropriate management and treatment.”
A cult in every sense of the word.
So let’s see for ourselves what exactly these austere authors are suggesting is worth the amazing benefits of vaccination, by reviewing case reports of graft rejection.
Vocabulary:
Keratoplasty = transplant
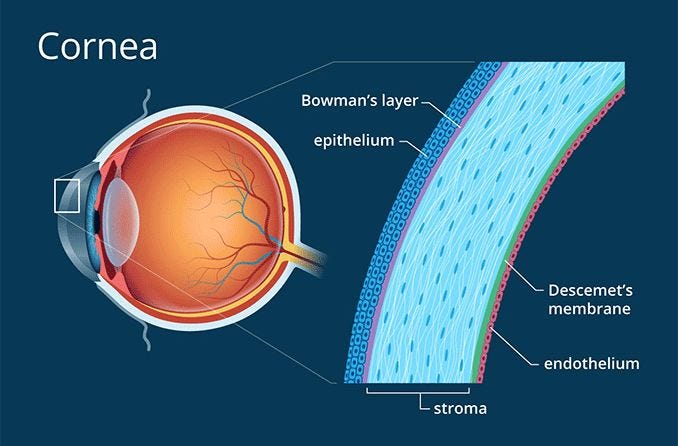
Descemet membrane endothelial keratoplasty / DMEK = “a method of corneal transplantation. The DMEK technique involves the removal of a very thin sheet of tissue from the posterior side of a person's cornea, replacing it with the two innermost layers of corneal tissue from a donor's eyeball. The two corneal layers which are exchanged are the Descemet's membrane and the corneal endothelium.” (Wikipedia)
1. Acute corneal endothelial graft rejection following COVID-19 vaccination
https://pubmed.ncbi.nlm.nih.gov/34281760/
Vaccine: Pfizer, Dose 1
A 71-year-old male patient with a history of high blood pressure, smoking, coronary artery disease and endothelial decompensation after phacoemulsification underwent DMEK of the right eye.
Five months after surgery, the patient presented to the eye clinic for a sudden painless decrease of vision in the right eye that started on the morning of his presentation to our department.
On further questioning it was revealed that he received his first dose of the BNT162b2 mRNA SARS-CoV-2 (BioNTech/Pfizer) 7 days ago.
This we will discuss further in the series on “Vaccine Roulette”:
We discussed with the patient the possibility of an association between the first dose of vaccination and the acute transplant rejection. Given his history of cardiovascular risk factors, it was decided to move forward with the second dose of the vaccine while keeping him on topical steroids q2 h.
The patient received his second dose. The graft remained clear and the visual acuity remained stable three weeks after the second dose. It was decided at that point to taper the topical steroids progressively over four weeks to reach a maintenance dose of twice a day.
👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨
2. Acute Corneal Epithelial Rejection of LR-CLAL After SARS-CoV-2 Vaccination
https://pubmed.ncbi.nlm.nih.gov/34743101/
Vaccine: ? (it’s behind a paywall)
A 27-year-old woman developed acute epithelial rejection of LR-CLAL 2 weeks after receiving the SARS-CoV-2 vaccine. She received the LR-CLAL transplant 4 years and 7 months previously and had a stable clinical course with no history of rejection.
The novel SARS-CoV-2 vaccine upregulates the immune system to produce an adaptive immune response. The SARS-CoV-2 vaccine may potentially be associated with increased risk of rejection in those with ocular surface transplants.
👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨
3. Acute Bilateral Descemet Membrane Endothelial Keratoplasty Graft Rejection After the BNT162b2 mRNA COVID-19 Vaccine
https://pubmed.ncbi.nlm.nih.gov/35444474/
Vaccine: Pfizer, Dose 1
This poor woman lost both her corneal transplants:
We report a case of acute bilateral Descemet membrane endothelial keratoplasty (DMEK) rejection two weeks following BNT162b2 mRNA COVID-19 vaccine (Pfizer-BioNTech), reflecting on possible changes to the management of patients with DMEK scheduled for COVID-19 vaccination.
A 94-year-old woman with Fuchs’ endothelial dystrophy who underwent DMEK 24 months earlier (right eye) and 20 months earlier (left eye) demonstrated bilateral graft rejection two weeks after the first dose of COVID-19 vaccine.
Treatment was with dexamethasone/tobramycin six times daily. Poor response resulted in re-DMEK transplantation, starting in the left eye. At one-month follow-up, BCVA and CT were 0.5 and 538µm right eye and 0.63 and 504µm left eye.
We report the first acute bilateral DMEK graft rejection after a single dose of COVID-19 vaccine. We recommend clinicians exercise vigilance and consider dexamethasone 0.1% during the vaccination period.
👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨
4. A case of delayed inflammatory filler reaction following vaccination with succesful response to colchicine
https://pubmed.ncbi.nlm.nih.gov/34407723/
Vaccine: ? (it’s behind a paywall)
A 43-year-old female patient treated with HA fillers developed an inflammatory reaction following vaccination in all areas of injection, including temples, lips, and lower eyelids. Systemic steroid and ciprofloxacin were used as a first-line treatment without response. Colchicine 1 mg/day along with hyaluronidase in lower eyelids improved all lesions successfully.
👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨
5. Five Cases of Corneal Graft Rejection After Recent COVID-19 Vaccinations and a Review of the Literature
https://pubmed.ncbi.nlm.nih.gov/35383622/
Vaccine:
Pfizer, Dose 1
Pfizer, Dose 1
AZ, Dose 2
AZ, Dose 2
Pfizer, Dose 1We describe 5 cases—2 patients with Descemet stripping automated endothelial keratoplasty (for Fuchs endothelial dystrophy) who presented with acute corneal graft rejection after their first dose of mRNA (BNT162) vaccine. The other 3 patients who had penetrating keratoplasty performed more than 10 years ago for keratoconus presented with acute graft rejection—2 patients after their second dose of adenovirus vector (AZD1222) vaccine and 1 patient after first dose of mRNA (BNT162) vaccine. Three patients were not using any topical steroid treatment at the time of diagnosis of graft rejection. The mean duration between vaccination and onset of symptoms was 16.86 ± 6.96 days for the mRNA vaccine and 17 ± 11.89 days for the adenovirus vector vaccine.
Corneal graft rejection has recently been reported after COVID-19 vaccination. Patients with keratoplasty need to be advised regarding the risk of corneal graft rejection and warning symptoms of rejection after COVID-19 vaccination. Seeking early referral to the emergency department and increasing topical steroids pre–COVID-19 and post–COVID-19 vaccination may reduce the risk of rejection.
“Patients with keratoplasty need to be advised regarding the risk of corneal graft rejection and warning symptoms of rejection after COVID-19 vaccination”
👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨
6. A case of acute endothelial corneal transplant rejection following immunization with ChAdOx1 nCoV-19 coronavirus vaccine
https://pubmed.ncbi.nlm.nih.gov/35502082/
Vaccine: AZ, Dose 1
A 28-year-old female who underwent an uneventful femtosecond laser enabled keratoplasty (FLEK) in her left eye presented with pain, redness, and blurring of vision in the operated eye two weeks after getting immunized with COVID-19 vector vaccine (ChAdOx1 nCoV19 Vaccine Recombinant COVISHIELD, AstraZeneca).
The patient was diagnosed with acute corneal graft rejection and advised hourly topical steroids with cycloplegics and oral steroids. The patient responded to treatment and there was progressive reversal of graft rejection with the patient achieving best spectacle-corrected visual acuity (BSCVA) of 20/30 after five weeks of treatment. Our case highlights possible immune corneal graft rejection after COVID19 vaccination and the need to step up topical steroids before vaccination.
The ChAdOx1 nCoV-19 messenger RNA vaccine, however, uses a chimpanzee adenovirus (AZD1222 or ChAdOx1), which carries the SARS-CoV-2 spike protein. Following administration, the genetic material of the part of coronavirus is expressed which stimulates an immune response. Despite the immune privilege of the cornea, immune-mediated corneal allograft rejection can occur, especially after penetrating keratoplasty due to breakdown in the blood aqueous barrier.
Thus, there is a possibility of immune corneal graft rejection after COVID 19 vaccination even 11 years post penetrating keratoplasty. Timing the second dose of vaccination in patients presenting with rejection as well as the need for pre-vaccination immunosuppression regimen in high-risk eyes is equally important. We suggest starting corneal graft recipients on topical corticosteroids or stepping up the topical steroids at least 1 week before taking the vaccine to suppress the immune response and bring down chances of graft rejection. We also advocate informing the patients with corneal transplant to follow-up immediately after the vaccination to look for any signs of graft rejection.
How about informing patients it might be best to forgo vaccination altogether?
👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨
7. Dual Corneal-Graft Rejection after mRNA Vaccine (BNT162b2) for COVID-19 during the First Six Months of Follow-Up: Case Report, State of the Art and Ethical Concerns
https://pubmed.ncbi.nlm.nih.gov/34835205/
Vaccine: Pfizer, Dose 1
A 44-year-old Caucasian woman presented with a 2-day history of blurred vision, redness, and discomfort in her left eye, 13 days after receiving the first shot of the SARS-CoV-2 mRNA vaccine BNT162b2 (Comirnaty, Pfizer-BioNTech, Mainz, Germany).
At a 4-week follow-up, a further episode of rejection in her left eye was observed, in parallel with persistence of vitamin D deficiency (serum [25(OH)D] of 19 ng/mL). The corneal clinical picture was similar to previous episode. Steroid drops were re-started, and higher doses of vitamin D were prescribed (50,000 IU of vitamin D three times weekly). The corneal inflammation regressed in four weeks, and at six-months of follow-up, no further rejection episodes were observed.
Kudos to the patient’s GP, whoever he or she is:
Nonetheless, in agreement with her GP, the patient refused to receive the second dose of the vaccine.
“Nonetheless”
Makes it sound like the authors beg to differ…
Although it is difficult to demonstrate the causality between COVID-19 vaccine and corneal graft rejection, our case shows a temporal association between the two events. Moreover, a series of issues and criteria described in the specific guidelines (Causality Assessment of an Adverse Event Following Immunization—AEFI) suggests that this rare adverse event is likely due to immunization through a number of pathophysiological pathways.
A “number of pathways”, eh? We were told that there wasn’t even *ONE* plausible mechanism for the vaccines to cause severe adverse events, let alone “a number of pathways”.
👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨
8. Acute graft rejection in a high-risk corneal transplant following COVID-19 vaccination: A case report
https://pubmed.ncbi.nlm.nih.gov/34827040/
Vaccine: Pfizer, Dose 1
A 35-year-old Indian male laborer presented with an acute onset of diminished vision in his left eye (LE) since 2 days. He had history of taking the first dose of COVID-19 vector vaccine (ChAdOx1 nCoV-19 Corona Virus Vaccine Recombinant, COVISHIELD™) 4 days prior. He had undergone a repeat penetrating keratoplasty (re-PK, donor cornea size 7.5 mm) in his LE 6 months back after having a failed large graft (size not known) post therapeutic PK 3 years ago at another center.
Anticipating the second dose of the COVID-19 vaccine, the patient was advised consultation with an immunologist for systemic nonsteroidal immunosuppression for prophylaxis.
To conclude, as the COVID-19 pandemic and the COVID-19 vaccination drive are still on, corneal surgeons need to be aware of the possibility of acute graft rejection following vaccination. Patients awaiting optical CT should schedule a timeline of vaccine ahead of transplant surgery. Simultaneously, patients with CT need to be sensitized about post vaccination rejection episodes as timely diagnosis and prompt topical &/or systemic management of an acute graft rejection as observed in present case is important to prevent graft failure especially in HR category.
What we really need are doctors with a functioning prefrontal cortex.
👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨
9. Characteristics of endothelial corneal transplant rejection following immunisation with SARS-CoV-2 messenger RNA vaccine
https://pubmed.ncbi.nlm.nih.gov/33910885/
Vaccine: Pfizer Dose 1, Pfizer Dose 2
A 66-year-old woman with Fuchs endothelial corneal dystrophy (FECD) and a unilateral Descemet's membrane endothelial keratoplasty (DMEK) transplant received COVID-19 mRNA vaccine BNT162b2 14 days post-transplant. Seven days later, she presented with symptoms and signs of endothelial graft rejection. An 83-year-old woman with bilateral DMEK transplants for FECD 3 and 6 years earlier developed simultaneous acute endothelial rejection in both eyes, 3 weeks post second dose of COVID-19 mRNA vaccine BNT162b2. Rejection in both cases was treated successfully with topical corticosteroids.
All’s well that ends well?
👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨
10. Stromal rejection in penetrating keratoplasty following COVID-19 vector vaccine (Covishield) - A case report and review of literature
https://pubmed.ncbi.nlm.nih.gov/34937268/
Vaccine: AZ Dose 2
A 79-year-old single eyed patient presented with diminution of vision of one-week duration in the left eye. He had taken his second shot of COVID-19 vector vaccine (COVISHIELD) 6 weeks ago prior to the onset of symptoms.
The graft had a localized central stromal edema suggestive of a stromal rejection.
Considering his single-eyed status, he was started on hourly topical steroids along with oral steroids, which were tapered gradually. At 2 months review, BCVA maintained at 20/120, edema resolved with a mild residual stromal haze [Fig. 2].
Ours is probably the first case of stromal rejection following COVID-19 vaccination. Like in all previous reports, we can only speculate that this is vaccine related as the patient was systemically stable and there were no ocular risk factors.
👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨
11. Corneal graft rejection after COVID-19 vaccination
https://pubmed.ncbi.nlm.nih.gov/34146066/
Vaccine: AZ Dose 1
A 62-year-old man presented with corneal graft rejection after COVID-19 vaccination. He had undergone penetrating keratoplasty for a childhood corneal scar in his right eye, 2 years ago.
He presented with congestion and diminution of vision of 5 days duration, having taken his first shot of COVID-19 vector vaccine (ChAdO × 1 nCoV-19 Corona Virus Vaccine Recombinant COVISHIELD™), 3 weeks prior.
There was an advancing horizontal Khodadoust’s rejection line in the center of the endothelium with graft edema at its wake inferiorly [Fig. 1] and grade 2 anterior chamber reaction. The graft superior to the rejection line was clear [Fig. 2]. Treatment for corneal allograft rejection was started. This may be the first report of graft rejection after COVID-19 vector vaccination.
👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨
12. Acute Corneal Transplant Rejection After COVID-19 Vaccination
https://pubmed.ncbi.nlm.nih.gov/34620770/
Vaccine: Moderna Dose 1, Moderna Dose 2, Moderna Dose 2, Moderna Dose 2
Four patients with prior keratoplasty developed presumed immunologic rejection after the mRNA-1273 vaccination for coronavirus 2 (SARS-CoV-2).
Case 1 had received Descemet membrane endothelial keratoplasty 6 months ago and presented with endothelial graft rejection 3 weeks after the first vaccine dose.
Case 2 had undergone penetrating keratoplasty 3 years previously and presented with acute endothelial rejection 9 days after the second vaccine dose.
Case 3 had prior Descemet stripping automated endothelial keratoplasty (DSAEK) and began experiencing symptoms of endothelial graft rejection 2 weeks after the second vaccine dose.
Case 4 presented with endothelial rejection of the penetrating keratoplasty graft 2 weeks after the second vaccine dose.
👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨
13. Keratoplasty Rejection After the BNT162b2 messenger RNA Vaccine
https://pubmed.ncbi.nlm.nih.gov/34029238/
Vaccine: Pfizer Dose 1, Pfizer Dose 1
Two men, aged 73 and 56 years, with a history of penetrating keratoplasty due to keratoconus were noted to have acute corneal graft rejection 2 weeks after receiving a first dose of the BNT162b2 mRNA vaccine. Both patients were treated with hourly dexamethasone 0.1% and oral prednisone 60 mg per day with prompt resolution of keratoplasty rejection.
Patient 1
A 73-year-old man presented with discomfort in his left eye 13 days after receiving a first dose of BNT162b2 vaccine. Ocular history included penetrating keratoplasty (PKP) in this eye due to keratoconus (1977) and regraft (2019) due to late endothelial failure. Medical history was unremarkable. The patient was maintained on 1 drop of dexamethasone 0.1% daily. A clear corneal graft was documented 2 months before admission. On presentation, corrected distance visual acuity decreased from 20/80 to 20/200. On biomicroscopy, ciliary injection, corneal edema, Descemet folds, and keratic precipitates (KPs) were noted (Fig. (Fig.1A).1A). A diagnosis of corneal graft rejection was made.
Patient 2
A 56-year-old man presented with a 2-day history of blurred vision and redness of the right eye, 14 days after receiving a first dose of the BNT162b2 vaccine. Medical history was unremarkable. Ocular history included keratoconus, with bilateral PKP performed 25 and 7 years before in the right and left eyes, respectively.
Diffuse corneal edema, KPs, and anterior chamber (AC) cells were noted on slit lamp biomicroscopy, indicating corneal graft rejection.
👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨
14. Acute Corneal Transplant Rejection After Severe Acute Respiratory Syndrome Coronavirus 2 mRNA-1273 Vaccination
https://pubmed.ncbi.nlm.nih.gov/34690266/
Vaccine: Moderna Dose ? (Paywall)
A 51-year-old man with a history of keratoconus and penetrating keratoplasty underwent repeat penetrating keratoplasty for graft failure. The patient had an uncomplicated intraoperative and postoperative course with improved vision and a healthy graft. The patient received the SARS-CoV-2 Moderna vaccine on postoperative week 3, and within 3 days, the patient began developing eye pain, photophobia, and blurred vision. The patient was found to have graft rejection with corneal edema and endothelial keratic precipitates. The rejection did not improve despite a trial of increased topical steroids and ultimately evolved into graft failure.
👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨
15. Keratoplasty rejection after messenger RNA vaccine (BNT162b2) for COVID-19
https://pubmed.ncbi.nlm.nih.gov/35918988/
Vaccine: Pfizer Dose 1
This report shows a case of corneal transplant rejection after vaccination against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), short after receiving the BNT162b2 vaccine, in a patient who had undergone keratoplasty more than 20 years ago, with no previous episodes of rejection and no other factor that could lead to the findings on his examinations. After treatment with high doses of topic, oral, and sub-conjunctival corticoids, the patient had a favorable therapeutic response. The signs of corneal transplant rejection must be oriented to the patients and the causing factors actively searched by ophthalmologists so that treatment is rapidly initiated and sequels are avoided. This report raises the question if these events are correlated and whether the patient should receive the second dose of the vaccine against SARS-CoV-2 or not.
Yeah, that should be an easy question.
Unfortunately, given the track records of most docs……
👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨
16. Corneal graft rejection following COVID-19 vaccine
https://pubmed.ncbi.nlm.nih.gov/34426655/
Vaccine: Pfizer Dose 1
In February 2021, a 68-year-old woman attended the eye casualty with a 1-day history of left painful red eye and rapid deterioration of vision. Four days earlier, she received her first dose of mRNA-based BNT162b2 COVID-19 vaccine (Pfizer-BioNtech). On the next day, she developed moderate systemic reactions, including chills, myalgia, and tiredness, followed by unexpected ocular symptoms on the third day.
The patient was immediately treated with hourly topical dexamethasone 0.1% and a week of oral acyclovir 400 mg 5x/day (to cover for any possible underlying herpes simplex keratitis), with no treatment modification in the right eye. Significant improvement was noted by 3-week post-treatment with complete resolution of corneal graft rejection (Fig. 1C, D).
The authors of this study had some eye-opening (pun intended) thoughts on the matter:
Discussion
Corneal graft rejection after vaccination is rare, with most evidence so far being linked to influenza vaccination. To our best knowledge, this is the second report of corneal allograft rejection following COVID-19 vaccine [4].
COVID-19 vaccines have been shown to induce SARS-CoV-2 neutralising antibodies and elicit strong Th1-biased CD4+ responses in human [3]. CD4+ Th1 cells have been shown to be the main mediators of corneal graft rejection [5], which could have contributed to the graft rejection. Intriguingly, corneal graft rejection only occurred in the left eye despite the presence of bilateral grafts. This may be attributed to the more recent history of left eye surgery and a repeat graft, which is known to have a higher risk of rejection. Although a direct cause-and-effect relationship remains to be established, it would be prudent to defer elective corneal transplant by 3–6 months after the second dose of COVID-19 vaccines and to consider institution of intensive topical steroids (6–8 times a day) in grafted eyes at the time of the first dose of vaccine until at least a month after the second dose, as the immune response peaks on 7–28 days post vaccine [3].
👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨👁👁🗨
Bonus:
There are a few more case reports of covid infection leading to rejection of eye grafts or transplants. This suggests that the reports of similar rejections occurring shortly after vaccination are indeed attributable to the vaccines, which share the primary features of the covid virus responsible for causing these injuries.
Acute Endothelial Graft Rejection Following COVID-19 *Infection*
https://pubmed.ncbi.nlm.nih.gov/34722015/
Here, we report a case of acute endothelial graft rejection following coronavirus disease 2019 (COVID-19). A 57-year-old woman who underwent therapeutic penetrating keratoplasty for a perforated infectious corneal ulcer in her right eye developed severe acute respiratory syndrome coronavirus 2 infection, which required intensive care and treatment with steroids. Acute endothelial graft rejection was seen at three weeks postoperatively and managed with high-dose corticosteroids. Despite standard therapy, secondary graft failure was observed. Immune dysregulation associated with COVID-19 may be a significant cause of acute endothelial graft rejection among keratoplasty patients with COVID-19.




Jabbed can't win for losing. It suppressed their immune system to make them infection and cancer vulnerable yet probably unleashes enough of a cytokine storm to cause this.
Thanks for this post. I was really disturbed by people getting kicked off transplant lists. I wonder if other transplant organs are having the same problem, and if not, why? I've heard of an unusual amount of harm to the eye from the vaccine where people have to have their eye removed, maybe eye cancer? So there's something about the eye region that seems to attract this vaccine injection spike.
It's also disturbing that the scientists need to pay homage to pharmaceutical companies in governments by continuing to explicitly recommend their product.